“`html
Effective Methods for How to Get Rid of Fungal Acne in 2025


Understanding Fungal Acne Symptoms
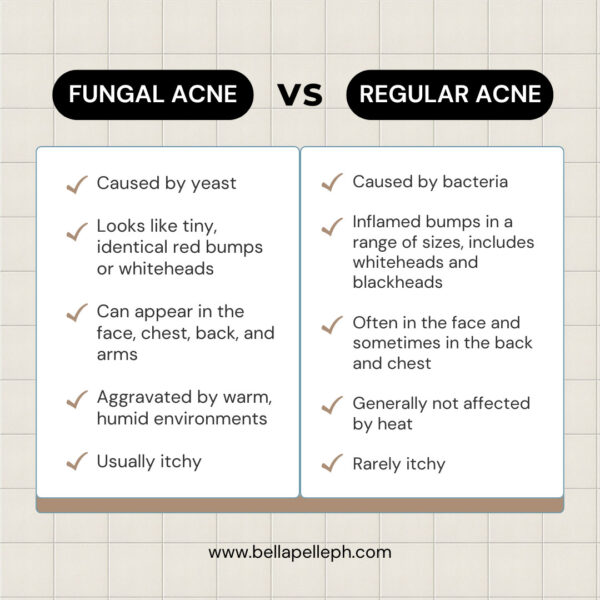
Fungal acne can often be mistaken for regular acne due to its similar appearance. **Fungal acne symptoms** usually include small, itchy red bumps that can occur on various parts of the body, like the face, chest, and back. These pustules are often uniform in size and may be accompanied by a rash. Identifying the difference between *fungal acne vs regular acne* is crucial for correct treatment. Unlike cystic acne, which typically consists of larger, painful lumps, fungal acne is often more superficial and can be exacerbated by humidity and heat. To effectively treat fungal acne, it’s essential to understand its characteristics and how it manifests on the skin.
Fungal Acne vs Regular Acne
The primary distinction between fungal acne and regular acne lies in their origins. Fungal acne, or *yeast acne*, is caused by an overgrowth of Malassezia yeast that naturally resides on the skin. This can be triggered by excess oil, sweat, and certain conditions that favor yeast growth. In contrast, traditional acne is primarily caused by clogged pores due to oil, dead skin cells, and bacteria. Understanding these factors can guide you in your journey toward finding the most effective *fungal acne treatments*.
Identifying Fungal Acne Signs
Recognizing the signs of fungal acne is vital for choosing the right *fungal acne solution*. Symptoms include persistent itchiness, a rash-like appearance, and the lack of blackheads typically associated with regular acne. A dermatological evaluation is often recommended for accurate *fungal acne diagnosis*, as many individuals misidentify their condition. Implementing proper techniques to identify and differentiate fungal acne from other skin conditions may include examining the distribution of pimples and their response to different treatments.
Common Causes of Fungal Acne
Understanding the *fungal acne causes* is essential to prevent recurrence. Common triggers include excessive sweating, wearing tight or non-breathable clothing, and frequent use of heavy, occlusive skincare products. Additionally, antibiotic use can disrupt the skin’s microbiome and provide an opportunity for fungal growth. Consider integrating lifestyle changes focused on moisture management and specific cleaning routines to help avoid conditions that contribute to fungal acne. This includes wearing moisture-wicking clothing and ensuring regular cleansing of the skin’s surface to eliminate excess oils.
Fungal Acne Treatment Options
When it comes to effective *fungal acne treatment*, a variety of methods can be explored, including topical and oral antifungal medications, as well as natural remedies. Choosing the right products can significantly influence both the speed and success of the healing process. Topical treatments such as antifungal creams or *antifungal shampoo for acne* can help eliminate the yeast responsible for the breakouts. In severe cases, dermatologists may recommend oral antifungal medications. By crafting a personalized *skincare routine for fungal acne*, not only can you treat existing conditions, but you’ll also help prevent future outbreaks.
Topical Antifungals for Acne
Among various therapeutic options, topical antifungal treatments play a crucial role in combating fungal acne. These include products containing agents like ketoconazole, clotrimazole, or ciclopirox—all effective in reducing the yeast population on the skin. It’s vital to apply these treatments as directed to maximize their effectiveness. Incorporating these products into your daily *skincare routine for fungal acne* could lead to significant improvement, often within a few weeks.
Oral Antifungal Medication for Acne
For those struggling with stubborn fungal acne, dermatologists may advocate the use of oral antifungal medications. This option is typically explored when topical treatments fail to yield results. Oral treatments like fluconazole target fungal infections from within and can effectively reduce fungal acne significantly. However, it is crucial to consult a healthcare professional to discuss potential side effects and the ideal treatment duration to achieve optimal outcomes in overcoming these persistent flare-ups.
Natural Remedies for Fungal Acne
Using *natural remedies for fungal acne* can be a gentle way to approach treating the condition. Ingredients like tea tree oil are celebrated for their antifungal properties and can be incorporated into your routine. Additionally, aloe vera and apple cider vinegar may also help soothe inflammation associated with fungal acne. Remember to perform a patch test when trying out new natural solutions to avoid any allergic reactions. Pairing these remedies with your existing skincare regimen can promote healing while providing skin the necessary care it needs to manage yeast effectively.
Skincare Products for Fungal Acne
Selecting the best products for fungal acne is essential to ensure your skin remains balanced and free from triggers. Many popular skincare items contain pore-clogging ingredients or excessively high levels of oils, which can exacerbate fungal growth. Look for *fungal acne skincare products* that are non-comedogenic and contain antifungal ingredients. Regularly using a *face wash for fungal acne* specifically designed for the condition can be a game-changer in managing both oil production and yeast levels on your skin.
Skincare Ingredients for Fungal Acne
When choosing *skincare ingredients for fungal acne*, opt for formulations that feature salicylic acid, glycolic acid, or benzoyl peroxide, all of which can help with oil control. Additionally, substances with proven antifungal capacities, such as azole antifungal ingredients, are good candidates for targeting yeast-related concerns. Prioritizing a product that supports the skin barrier while managing excess oil and hydration can lead to skin recovery, decreased recurrence of fungal acne, and improved overall skin health.
Proper Cleansing Methods
A proper cleansing method is critical in addressing fungal acne effectively; this involves using a gentle foaming cleanser containing antifungal properties. Daily **cleansing routines for fungal acne** must balance removing impurities and maintaining skin hydration. After cleansing, always follow up with a light moisturizer to enhance skin barriers. Avoid heavy creams or oil-based products that can foster a thriving environment for fungi. Building a consistent, effective cleansing regimen will be essential for long-term results.
Preventing Fungal Acne
Preventing fungal acne requires changes in both lifestyle and skincare habits. Implementing *fungal acne prevention techniques* can significantly contribute to healthier skin. Strategies to consider include wearing breathable clothing, practicing good hygiene, and minimizing exposure to humid environments. Moreover, if you notice recurrent *fungal acne flare-ups*, reassessing your skincare products and diet can be beneficial in maintaining clear skin. Including *oral probiotics for skin health* may further enhance your skin’s defenses against fungal colonization.
Key Takeaways
- Identifying fungal acne symptoms accurately is crucial for effective treatment.
- There are various tailored treatment options, from topical to natural remedies.
- Selecting the right skincare products is essential to avoid clogging pores.
- Implementing lifestyle changes can minimize the risk of fungal acne re-emergence.
- Consulting with dermatologists can provide personalized skincare strategies.
FAQ
1. What are the most effective fungal acne treatments?
The most effective fungal acne treatments often include topical antifungal medications like ketoconazole and clotrimazole, as well as oral medications for severe cases. Incorporating antifungal shampoos and natural remedies like tea tree oil can also be beneficial in managing the condition.
2. Can diet impact fungal acne?
Yes, your diet can influence fungal acne. Foods rich in sugar and refined carbohydrates may encourage yeast overgrowth, so it’s wise to modify your diet towards whole foods and consider incorporating oral probiotics for skin health.
3. How can I differentiate fungal acne from other types of acne?
Fungal acne typically presents as small, itchy, and uniform red bumps without blackheads. It’s often located on oily areas simultaneously and may worsen in humid conditions. Consulting with a dermatologist for accurate diagnosis is recommended.
4. Are there specific skincare products to avoid with fungal acne?
Yes, avoiding products that are high in oils, glycerin, or other heavy ingredients is critical for those with fungal acne. Non-comedogenic and antifungal skincare formulations are recommended to minimize the risk of flare-ups.
5. Can stress lead to fungal acne outbreaks?
While stress itself does not directly cause fungal acne, it can lead to hormonal fluctuations that increase oil production, potentially creating an environment that facilitates fungal growth. Managing stress through healthy lifestyle changes can be beneficial.
“`